The stillbirth of a baby at Wexford General Hospital (WGH) four years ago could have been avoided, if doctors had delivered the boy at an earlier stage, given complications with his mother from a common condition in pregnant women, an inquest has heard.
A jury of six men returned a verdict of medical misadventure into the death of baby, Noah O’Shea-Rodgers, who was stillborn when delivered at WGH on 24 April 2020.
An expert witness, Professor Fergal Malone, criticised a number of elements in the care of the baby’s mother, Claire O’Shea, at the hospital including a delay of 15 minutes in deciding to deliver the baby via an emergency caesarean section, as well as earlier missed opportunities to diagnose her with preeclampsia and to manage the condition.
Preeclampsia is a medical condition linked to high blood pressure which can pose a serious risk to both mother and baby.
Lack of oxygen
A post mortem showed the baby had died as a result of lack of oxygen from a severing of the placenta which was caused by his mother’s preeclampsia.
Prof Malone, a former master of the Rotunda Maternity Hospital in Dublin, told a sitting of Wexford Coroner’s Court that there was no doubt that baby Noah would have been born alive in “perfectly healthy” condition if he had been delivered earlier, after his mother had demonstrated warning signs of severe preeclampsia the previous evening.
The consultant obstetrician and gynaecologist said it was obvious from a review of medical records that by 10 April 2020 or shortly thereafter that Ms O’Shea had preeclampsia.
However, the inquest heard it was only confirmed on 23 April 2020 at WGH, although she had been treated for high blood pressure for around a month.
Evidence was also heard that there was a delay of two days in confirming Ms O’Shea’s diagnosis with preeclampsia as certain laboratory tests could not be carried out at WHG.
Prof Malone said pregnant women with preeclampsia were normally admitted as inpatients until delivery but said Ms O’Shea had been regularly monitored as an outpatient at WGH.
He told a sitting of the coroner’s court in Gorey that scans carried out on Ms O’Shea up to 20 April 2020 had been reassuring, but her condition had begun to deteriorate by the following day when she had severe hypertension.
Prof Malone said the appropriate decision was made at the time to admit her to hospital and to give her steroids to help the development of her baby’s lungs for delivery.
He acknowledged there was a debate among medical professionals about when delivery was optimum in the case of women with severe preeclampsia.
However, he told the coroner, Seán Nixon, that the risk associated with the premature birth of a baby was relatively minor in Ms O’Shea’s case given she was almost 34 weeks into her pregnancy.
Prof Malone said delivery was generally recommended in cases where a mother with preeclampsia was also displaying neurological symptoms like headaches and blurred vision.
The inquest heard evidence that Ms O’Shea had reported experiencing both such conditions on the evening of 23 April 2020, but a decision was not made to carry out an emergency caesarean section until the following night.
‘Probably unwise’
Prof Malone said the delay by up to 24 hours in delivering the baby was “probably unwise” as doctors had enough information on 23 April 2020 to arrange a non-emergency delivery for Ms O’Shea.
The consultant acknowledged the appropriate decision to carry out an emergency caesarean section was taken around 10.40pm on 24 April 2020 after the baby’s heartbeat started to deteriorate and was performed within an impressive 13 minutes.
He also noted that it was easier to make decisions about a patient’s care from medical records than in real time.
Pathologist, Dr John Gillan confirmed that the baby’s death was linked to his mother’s preeclampsia.
Questioned by counsel for the baby’s parents, Doireann O’Mahony BL, Dr Gillan, said he believed the outcome could have been different if the baby had been delivered earlier.
A specialist registrar at WGH, Aoife McTiernan, said she could not recall if she had been told on 24 April 2020 about Ms O’Shea experiencing a headache and blurred vision the previous evening.
However, Dr McTiernan said she had been reassured herself by Ms O’Shea that she was not experiencing such symptoms when she examined her that morning.
The inquest heard a review into the baby’s death carried out by WGH had established a key factor as a delay in the baby’s delivery.
Dr McTiernan observed that medical staff were working “in an incredibly difficult situation”.
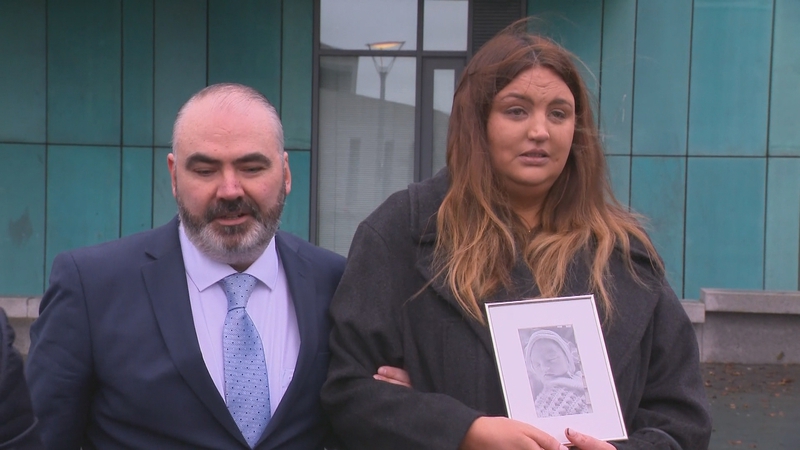
In a joint statement, the baby’s parents, Claire O’Shea and Shane Rodgers said they had learnt of her pregnancy shortly after they had become engaged in October 2019.
“We could not have been happier for the journey we were to begin together,” Mr Rodgers said.
The couple said they had alerted hospital staff that Claire had a family history of preeclampsia, while she also had elevated blood pressure at ante-natal appointments.
They said they were extremely hurt and angry that a diagnosis of preeclampsia was only made late in her pregnancy.
“We feel that if a diagnosis was made earlier and a plan put in place to manage the condition, Noah’s life may well have been saved,” Mr Rodgers said.
The couple said their first child was “a much wanted and much loved baby”.
Mr Rodgers complained that when his wife woke up in theatre and asked about Noah that a doctor replied rather abruptly: “He is dead Claire”, before walking away.
“This was already a very traumatic time for Claire and it was further compounded by the terrible attitude and choice of words used by the doctor,” Mr Rodgers said.
“Our lives have changed forever following Noah’s preventable death,” the couple noted.
“We have both suffered mentally and have required both individual and couple counselling to help deal with the consequences that Noah’s death had on us.”
They said they had also experienced a great strain on their relationship which they believed was solely due to their son’s death.
“Had Noah been cared for appropriately he would have been delivered safely and the mental health issues we continue to suffer from would have been prevented,” they said.
The couple who come from Summerhill, Wexford subsequently had another baby boy, Shay.
Verdict
The jury returned a verdict of medical misadventure and recommended that HSE guidelines on the diagnosis and treatment of pre-eclampsia be circulated to staff at WGH.
Dr Nixon said the verdict did not blame or exonerate anyone for baby Noah’s death and the coroner acknowledged it was a “very difficult and emotional” day for both the baby’s parents and hospital staff.
A solicitor for the hospital, Peter Groarke, said staff had already been reminded about the guidelines on pre-eclampsia.
Following the inquest, a solicitor for Noah’s parents, John Kelly said Noah’s death was “an absolute tragedy – a child deprived of life and parents deprived of their healthy child”.
“It is a tragedy that should not have happened and was preventable,” said Mr Kelly.
He said preeclampsia was a well recognised condition in pregnant women with well established guidelines for the management of the condition.
However, he said Ms O’Shea’s condition was negligently mismanaged.
Mr Kelly said the verdict justified their pursuit of the case since 2020 and more importantly it raised awareness among the public and medical staff so that someone with Ms O’Shea’s condition would “speak up louder” in future and question their medical treatment, while medical staff might listen more attentively to patients.
“Perhaps a life could be saved and a child may have the chance of life. Tragically for Shane and Claire, Noah wasn’t given that chance,” he concluded.
Source link
 TG4 TV PC to TV
TG4 TV PC to TV
