Finding the prescription for chronic overcrowding

Overcrowding has become such an endemic part of the health system, there is always the danger that some people may now view it as simply unsolvable.
It has been a part of the health service for decades but has become more chronic and ingrained.
At its most simplistic level, it is a way of managing capacity, meaning that when there are insufficient beds, patients must wait.
That is the same with hospital waiting lists for treatment.
But of course, overcrowding is more complex than that, because the severity of it is linked to having sufficient beds, staff, the right skills mix, good patient management and hospital governance built around safe, patient care.
Hospitals also need to be fully funded for their size and catchment area.
We see some hospitals perform very well with little or no overcrowding, like Waterford, while others like University Hospital Limerick are in the news daily, at times breaking records with overcrowding levels.
Each hospital is different and has its own challenges, and demographic profile.
The HSE provides official figures on hospital overcrowding each day. Likewise, the Irish Nurses & Midwives Organisation also provides its own figures.
While both sets of data often differ, they all show one thing – hundreds of patients waiting for admission to a bed each day.

There may be arguments about whether trends are going down or up, some months are better than in previous years, yet one patient waiting excessive hours for admission to a bed is one patient too many.
This is especially true when it involves older, frail patients.
The HSE target is that no more than 320 patients can be waiting for admission to a bed at 8am, each day, on average in a month.
It also commits to having no patient over 75 years waiting over 24 hours for admission to a bed.
On Friday, the HSE figures showed 331 patients waiting for admission to a bed nationally.
The INMO figure was slightly higher at 369.
According to the HSE figures, 254 patients were in emergency departments and 77 were on wards.
There were 51 patients waiting for admission to a bed for over 24 hours and 9 of these people were over 75 years.
This week, Limerick University Hospital has been a key focus of the impact of overcrowding.
The knock-on effect, in order to free up hospital beds, saw two days of cancellations for planned surgery at five hospitals in the group.
So, we can see that overcrowding also leads to longer waiting lists for planned procedures.
There are aspects particular to Limerick that are important to recognise.
In particular, the Health Information & Quality Authority (HIQA) report into its emergency department in 2022 explained it well.
It pointed to insufficient nurse staff levels, ineffective patient flow and the hospital was not organising nurse staff levels to ensure high-quality safe care.
During the HIQA visit inspectors found it had twice as many patients in the emergency department than the building was designed to hold.
We also know that UHL has a huge catchment area of over 400,000 people, covering Limerick city and county, Clare and north Tipperary.
The closure of the EDs many years ago at Nenagh and Ennis, which the HSE explained was for patient safety reasons, has obviously had an impact.
A new 96-bed block being built at University Hospital Limerick is not expected to be open for another year or so.
When it comes on stream it will ease the pressure.
Emergency medicine consultant at UHL, Dr Alan Watts, told RTÉ News this week that the hospital is experiencing “significant capacity issues” and he said it was the busiest emergency department in the country.
Dr Watts is also a member of the committee of the Irish Association for Emergency Medicine, and he said it was a reflection that nationally, bed capacity is significantly under capacity.

He noted that the OECD average for bed capacity is 4.3 per thousand population, whereas in Ireland it is 2.9 per thousand population, “which reflects a significant deficit in acute beds”.
The Government has added over 1,000 more beds to the hospital system.
In the Dáil, Sinn Féin leader, Mary Lou McDonald detailed the case of an elderly patient who was recently on a trolley in Limerick for eight days.
She warned that without urgent action the situation will get even worse.
Taoiseach Leo Varadkar acknowledged that staff are working under enormous pressure and patients are experiencing things they should not have to experience at UHL.
He said that in Limerick there is a particular challenge but the budget for the hospital had increased by 45% in the past four years and 1,000 more staff are now employed there.
This includes 140 more doctors and 45 more consultants, but the Taoiseach conceded that the problems at UHL are very real.
Bernard Gloster, Chief Executive of the Health Service Executive described delays in hospitals, particularly in Limerick, as unacceptable.
He added that in the first nine weeks of this year, attendances at emergency departments across the country had risen by just under 13% and Limerick by 16%.
“Those kinds of numbers do not mean anything to people when they are waiting but we have seen, certainly post-Christmas, a very significant change in attendances at hospital. That pushes us to look exactly at what we are doing in our hospitals but also outside in primary care and in the community, but certainly those types of numbers are not acceptable,” he said.
It appears that the difficulties being experienced by patients and staff in Limerick are likely to continue for some time.
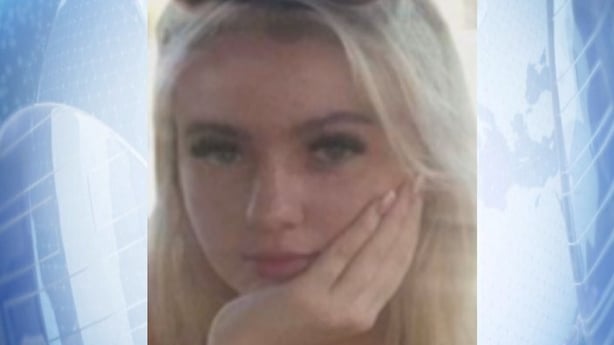
Separately, there is an ongoing independent investigation into the death of teenager Aoife Johnston at Limerick hospital in December 2022.
She died after a 12-hour wait in the emergency department and had been diagnosed with bacterial meningitis and developed sepsis.
That probe is being led by retired Chief Justice, Frank Clarke and is not expected to be completed for a few more weeks.
It is charged with looking at the circumstances of her death and the clinical and corporate governance at Limerick.
Overcrowding around the country can be exacerbated because some people are now experiencing long delays in getting an appointment to see their GP.
If they are concerned about their health condition, they may go to an emergency department, just to be safe.
HIQA looked at overcrowding generally two years ago.
It concluded that it compromises the dignity and respect of patients and poses a risk to health and safety of patients.
The health watchdog called for improvements to ensure that there is a balanced approach to the daily operational management of patient flow, capacity and appropriate staffing, which is clearly linked to patient safety and activity.
The four themes it identified for hospitals were:
– The need to continue to urgently build additional capacity within the whole healthcare system, both acute and community.
– A more effective approach to strategic workforce planning to better anticipate and manage staff shortages.
– More responsive leadership, governance and management arrangements at local, regional and national level which acts to address performance issues when identified.
– More effective identification, monitoring and management of patient safety risks associated with overcrowding in emergency departments.
HIQA warned that emergency department overcrowding and insufficient access to acute and primary services will continue to occur, unless a system-wide approach is taken to address major structural concerns and respond to, rather than continuing to tolerate or normalise, the problem.

So, the causes and solutions to overcrowding have been well documented.
Each week, we see quite a similar pattern. Usually on Mondays and Tuesdays, the largest number of patients are waiting for admission to a bed.
As each week progresses, the numbers decline, as patients are treated and discharged. Friday’s generally see the lowest number of patients waiting for admission to a bed.
At weekends, things often deteriorate as hospitals are not operating weekday services and there can be a build up of patients waiting to be discharged.
This means fewer beds for patients attending emergency departments.
The introduction of the new public-only hospital consultant contract has helped, with consultants rostered for the first time on Saturdays from 8am to 6pm.
Consultants can also be rostered to work an extended working day, Monday to Friday until 10pm.
This means senor decision making is available over a wider time period to have patients assessed, discharged and free up beds.
Even before the new contract offer, many consultants would be in hospitals at weekends, but the system is now formalised in rosters.
Over 1,900 consultants (45% of the consultant workforce) have moved over to the new contract which only came in a year ago, so that is progress.
The latest figures also show that 45% of emergency medicine consultants are now on this new public only contract.
This and other factors may be why we have not seen any new record numbers of overcrowding this year.
However, if the patient is supposed to be at the centre of everything that happens in the health system, the continuing cycle of high daily overcrowding needs to end for good.
The prescription is there.





